When Breast Cancer Doesn’t Start in the Breast
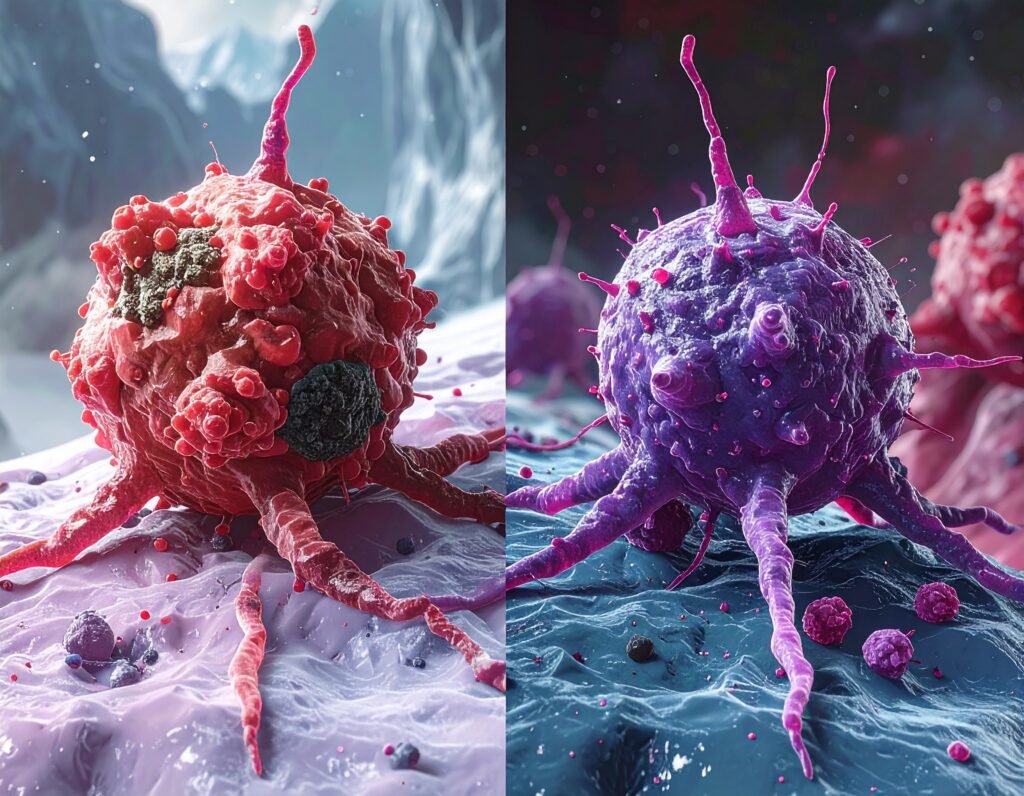
[wpr-template id=”4771″] When Breast Cancer Doesn’t Start in the Breast Sometimes breast cancer starts in lymph nodes before it’s visible in the breast. Discover how this rare “hidden” form challenges what we think we know. Breast Cancer Can Start Outside the Breast When we think of breast cancer, most of us picture a lump in […]